Sunday Poster Session
Category: Colon
P0374 - Subacute Pseudo-Obstruction in End-Stage Scleroderma Bowel Disease: Transition From Neostigmine-Induced Decompression to Oral Pyridostigmine

Lesline Martes, BS
Albany Medical Center
New Windsor, NY
Presenting Author(s)
Albany Medical Center, Albany, NY
Introduction:
Systemic sclerosis (SSc) is a chronic autoimmune disease characterized by progressive fibrosis and vascular dysfunction, often affecting the gastrointestinal (GI) tract. GI involvement most commonly presents with esophageal dysmotility and reflux. In rare, severe cases, the disease can evolve into end-stage scleroderma bowel disease with pseudo-obstruction, nutritional failure, and progressive colonic dysmotility. We present a case of a patient with diffuse SSc and multiple GI manifestations who developed sub-acute colonic pseudo-obstruction and was successfully managed with neostigmine and transitioned to oral pyridostigmine.
Case Description/Methods:
A 76-year-old woman with diffuse SSc complicated by pulmonary and pericardial effusions, severe GI dysmotility, and overlapping Sjögren’s syndrome presented with progressive abdominal distention and intolerance to enteral feeding. Her past history was also notable for esophageal dysmotility with recurrent infectious esophagitis, small intestinal bacterial overgrowth (SIBO), partial small bowel obstruction, and prior gastric volvulus requiring partial gastrectomy and long-term PEG tube placement. Over several months, she experienced worsening bloating despite erythromycin, osmotic laxatives, and dietary adjustments.
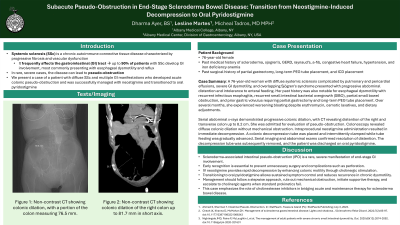
Serial abdominal x-rays demonstrated progressive colonic dilation, with CT revealing distention of the right and transverse colon up to 8.2 cm. She was admitted for evaluation of pseudo-obstruction. Colonoscopy revealed diffuse colonic dilation without mechanical obstruction. Intraprocedural neostigmine administration resulted in immediate decompression. A colonic decompression tube was placed and intermittently clamped while tube feeding was gradually advanced. Serial imaging and abdominal exams confirmed resolution of distention. The decompression tube was subsequently removed, and the patient was discharged on oral pyridostigmine.
Discussion:
SSc related pseudo-obstruction is a rare manifestation of GI involvement and while prokinetics and dietary adjustments are often first-line, patients with profound colonic dysmotility may require endoscopic intervention and different pharmacologic treatment. In this case, intravenous neostigmine produced immediate improvement, and oral pyridostigmine provided sustained benefit by enhancing cholinergic motility. This case highlights the importance of early recognition of pseudo-obstruction in SSc and the role of cholinergic agents when conventional oral therapies fail.

Disclosures:
Dharma Ayer, BS, Lesline Martes, BS, Micheal Tadros, MD. P0374 - Subacute Pseudo-Obstruction in End-Stage Scleroderma Bowel Disease: Transition From Neostigmine-Induced Decompression to Oral Pyridostigmine, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
