Sunday Poster Session
Category: Colon
P0375 - A Rare Case of Solitary Mesenteric Plexiform Neurofibroma
- PK
Pavit Kesar
Trinity University
San Antonio, TX
Presenting Author(s)
1Trinity University, San Antonio, TX; 2University of Texas Health San Antonio, Temple, TX; 3University of Texas Health San Antonio, Cleveland, OH; 4Gastro star / Solo provider/ practitioner., Shavano Park, TX; 5University of Texas Health San Antonio, San Antonio, TX
Introduction:
Mesenteric plexiform neurofibroma is a subtype of plexiform neurofibroma (PFN) affecting the mesentery that presents with gastrointestinal symptoms and is commonly associated with Neurofibromatosis Type 1 (NF1). We present a rare case of a young female with no NF1 diagnosed with solitary mesenteric PFN.
Case Description/Methods:
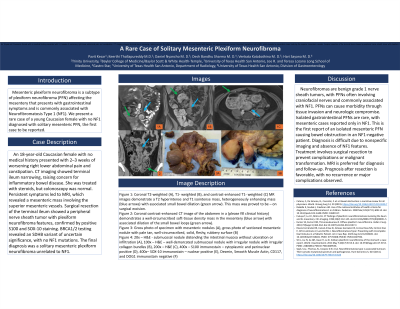
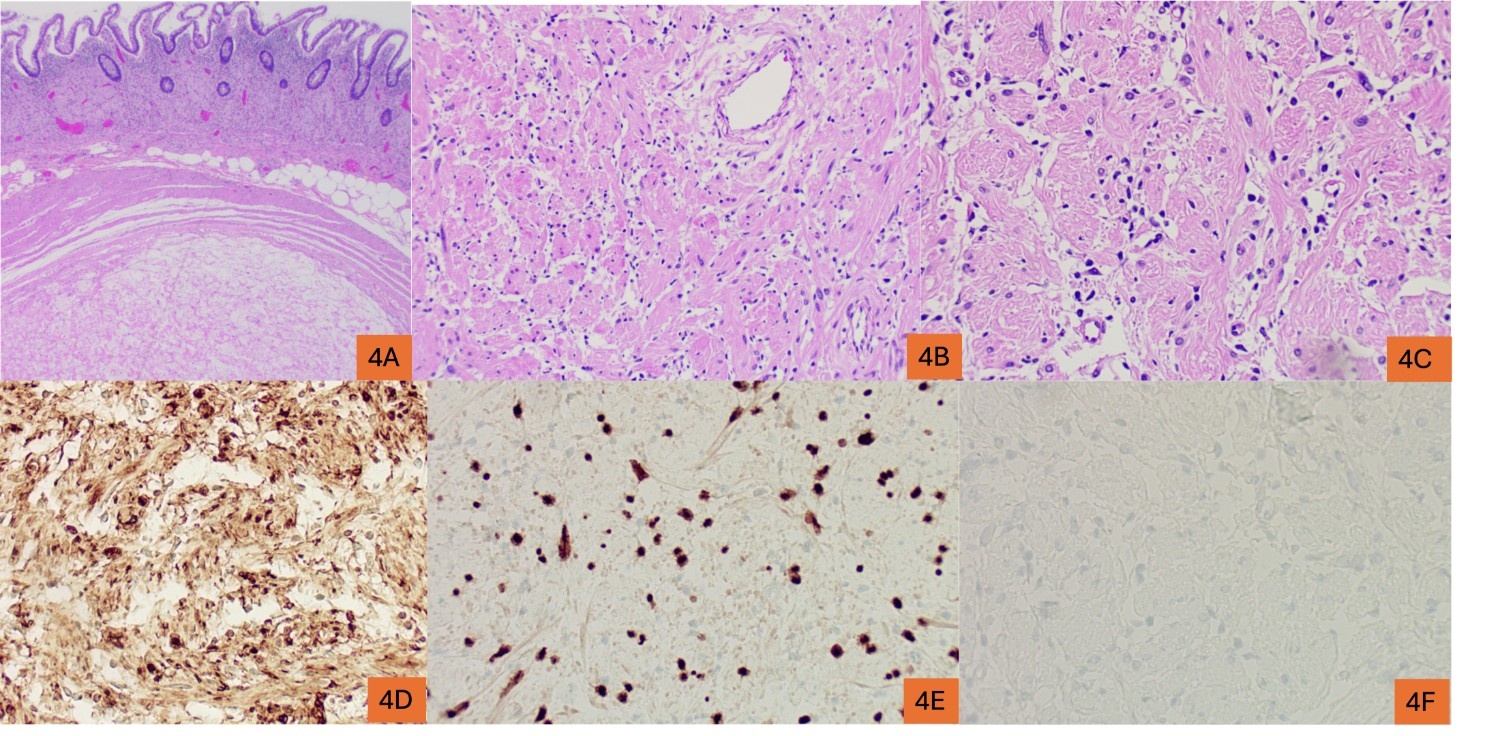
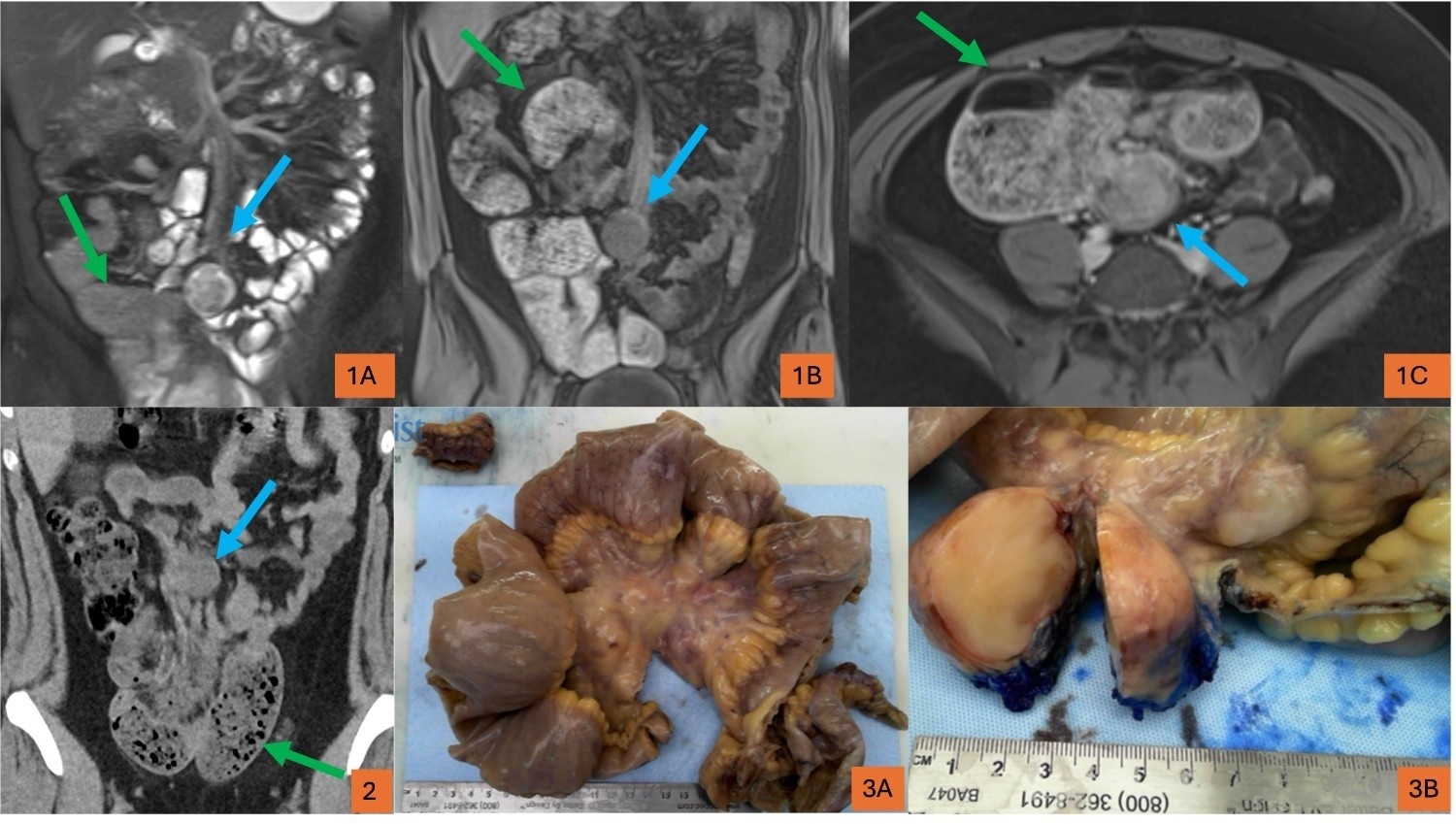
An 18-year-old Caucasian female with no prior medical history presented with worsening right lower abdominal pain and no bowel movements for 2–3 weeks. Initial imaging suggested terminal ileum narrowing, raising suspicion for inflammatory bowel disease. Despite steroid treatment and a normal colonoscopy, further imaging with MRI for persistent symptoms revealed a mesenteric mass involving the superior mesenteric vasculature. Surgical resection of the terminal ileum was performed, with histopathology showing a peripheral nerve sheath tumor with plexiform neurofibroma features, confirmed by positive S100 and SOX-10 staining. Genetic testing, including BRCA1/2 analysis identified an SDHB variant of uncertain significance, and was negative for NF1-associated mutations. The patient was ultimately diagnosed with a solitary mesenteric plexiform neurofibroma unrelated to NF1.
Discussion:
Neurofibromas are benign, grade 1 nerve sheath tumors classified into subtypes, including PFNs which often affect craniofacial nerves and are commonly linked to NF1. PFNs can cause significant morbidity through tissue invasion and neurological impairment. Solitary PFNs particularly in the gastrointestinal tract are rare, with mesenteric involvement previously reported only in NF1-associated cases. This case describes the first solitary mesenteric PFN causing bowel obstruction in an NF1-negative patient. Diagnosis can be challenging due to non-specific imaging findings and absence of typical NF1 features. Surgical resection remains the standard treatment to prevent complications and potential malignant transformation. MRI is preferred for diagnosis and monitoring due to superior soft tissue contrast. Prognosis after surgical resection is favorable, and typically with no recurrence or serious complications, as was seen this patient.
Disclosures:
Pavit Kesar, 1, Keerthi Thallapureddy, MD2, Daniel Nyancho, MD, BS3, Desh Sharma, MD4, Venkata Katabathina, MD5, Hari Sayana, MD5. P0375 - A Rare Case of Solitary Mesenteric Plexiform Neurofibroma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
